I really wish COVID weren't still such a relevant topic, but here we are. When I was given the opportunity to provide a comment or two on the topic of vaccination, especially my decision to be vaccinated while pregnant, my answer was an enthusiastic yes! It was even more enthusiastic when I was asked if …
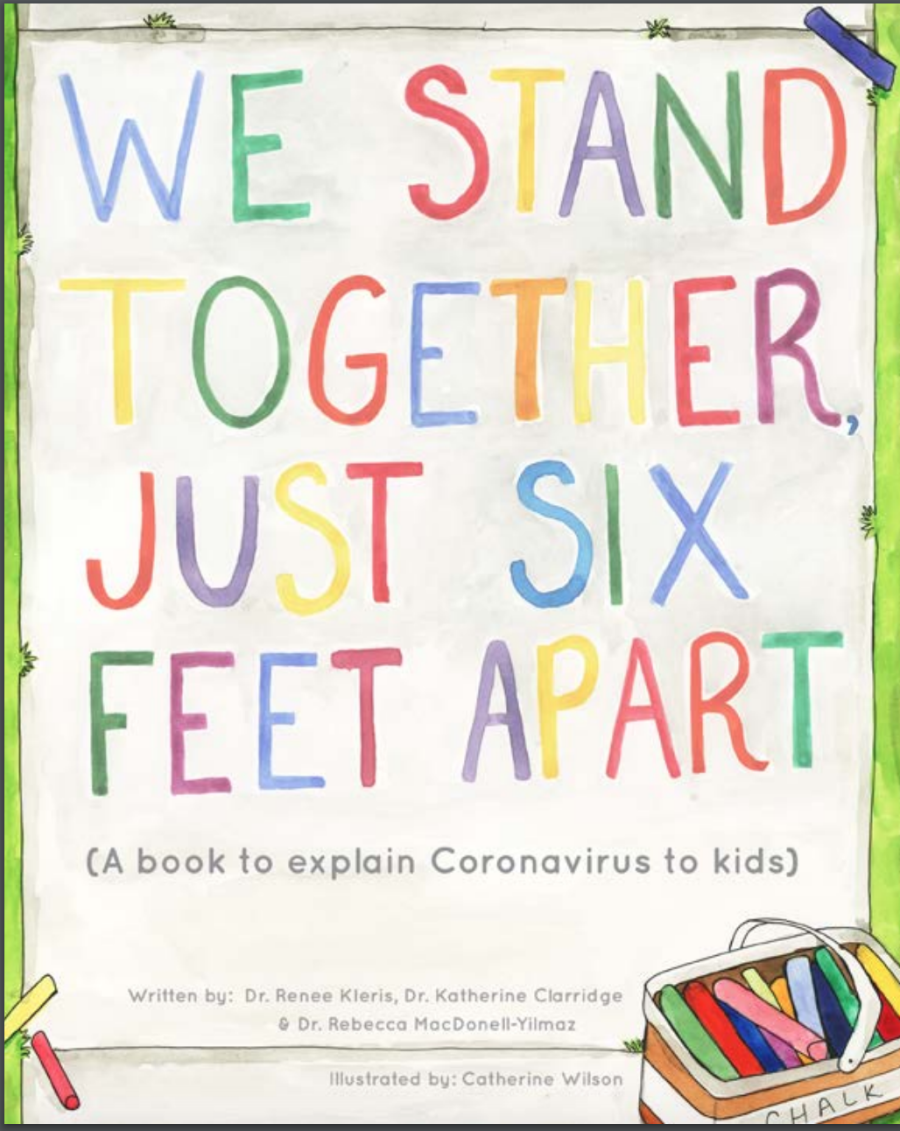
We Stand Together… Just Six Feet Apart
Publishing a children's book wasn't on my list of goals for 2020, but here we are! Several collaborators (an artist and two other physicians trained in pediatrics as well as allergy/immunology) and I joined forces this spring with the goal of developing a simple story to explain to young children why the world as we …
Physician Moms During COVID
What an honor to be invited to share my (and my colleagues') experiences as physician moms navigating the COVID pandemic! https://www.roshreview.com/blog/our-experiences-as-women-physicians-parents-coping-with-covid-19/
